Selecting management software involves strategic decisions that can boost ROI and operational efficiency.
Flexible plans are crucial as practices grow or change, impacting adaptability and cost-effectiveness.
Ease of data access and customizable reports are vital for informed decision-making and efficiency.
Seamless tech integration ensures operational continuity with existing tools like EHR and billing systems.
Industry-specific compliance with regulations like HIPAA is essential to avoid legal issues.
Choosing the right practice management software isn’t just a tech decision; it’s a strategic move. It can save you time, improve accuracy, and ensure compliance, all while boosting your return on investment. But choose poorly, and you risk wasted resources, frustrated staff, and compliance headaches.
This guide is for medical practice managers and team leads seeking to navigate these challenges. I’ll help you focus on what really matters to find software that supports your goals and needs.
9 Things to Look for When Choosing Practice Management Software
Evaluate practice management software by focusing on these key factors to ensure it aligns with your needs. Here's what to consider:
1. Plan Flexibility
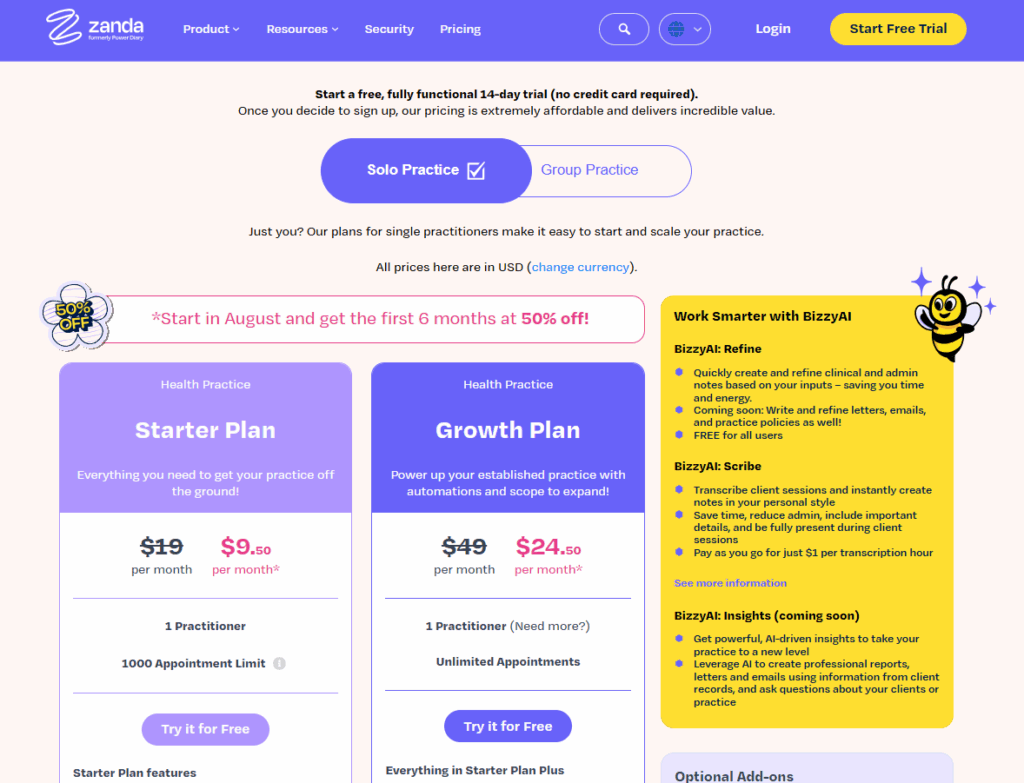
Plan flexibility means easily upgrading or downgrading your software as your needs change. It matters because your practice might grow or shift over time. Look for vendors that offer clear, straightforward options without hidden fees. Ask about their policy on changing plans and any associated costs. During a demo, inquire how quickly changes can be made.
2. Data Access and Reporting
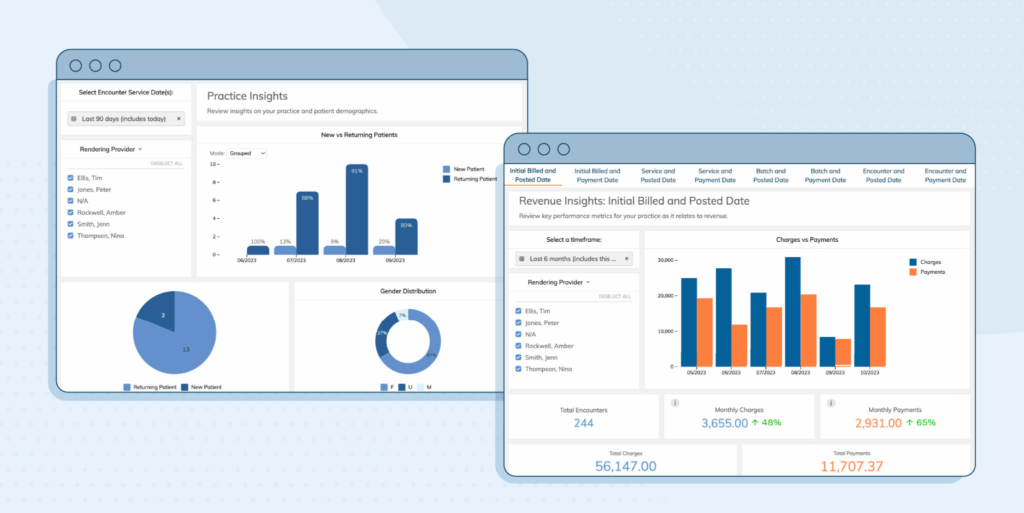
Good data access and robust reporting help you make informed decisions. You need software that provides easy access to patient data and generates useful reports. Check if the software lets you customize reports to fit your needs. During a trial, test how quickly you can pull up specific data and reports.
3. Integration with Your Tech Stack
Integration with your existing tech stack ensures seamless operations. Your practice management software should work well with other tools you use, like billing or electronic health records. Ask vendors for a list of supported integrations, and test these integrations during a demo to ensure smooth data flow.
4. Onboarding and Support
Onboarding and support are vital for a smooth transition. You want a vendor that offers comprehensive onboarding and ongoing support. Ask about their training resources and support channels. During a trial, contact their support to gauge response times and helpfulness.
5. Role-Based Permissions
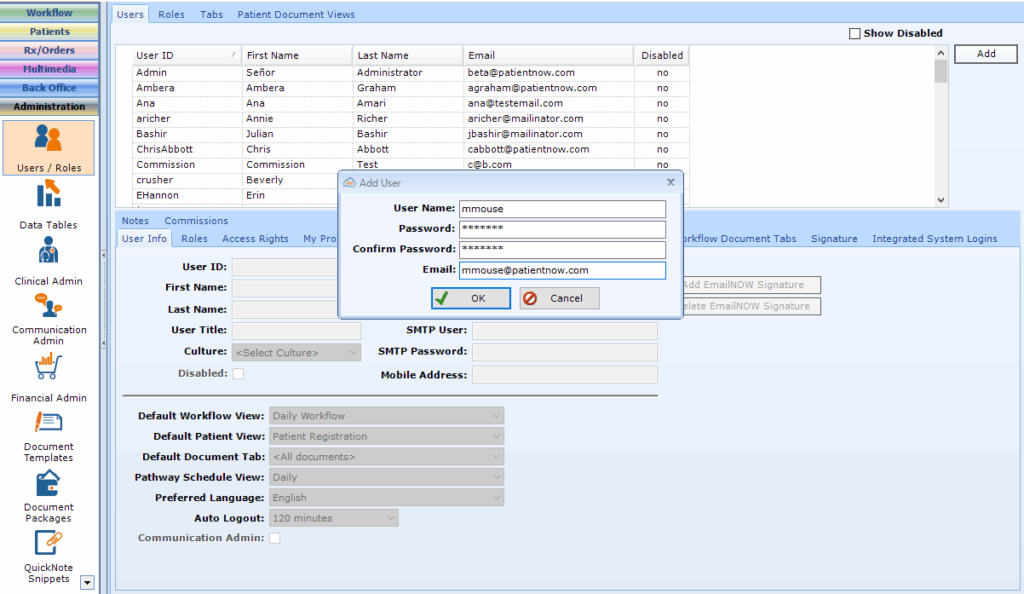
Role-based permissions help control who accesses what information. This is important for maintaining privacy and security. Look for software that allows you to set permissions based on roles within your team. Test this feature by assigning and modifying permissions during a demo.
6. Industry-Specific Compliance
Industry-specific compliance keeps your practice aligned with legal requirements. Choose software that meets healthcare regulations like HIPAA. Ask vendors how they handle compliance and request documentation. During a trial, review how the software manages compliance-related tasks.
7. Customization Options
Customization options let you tailor the software to fit your practice's unique needs. This flexibility can improve workflow efficiency. Check if the software allows you to customize features like templates and workflows. During a demo, try customizing a few elements to see how intuitive it is.
8. Automation Features
Automation features save time by handling repetitive tasks. Look for software that automates scheduling, billing, and reminders. Ask vendors what tasks their software can automate. During a trial, test an automated task to see how it functions and impacts your workflow.
9. Mobile or Multi-Location Support
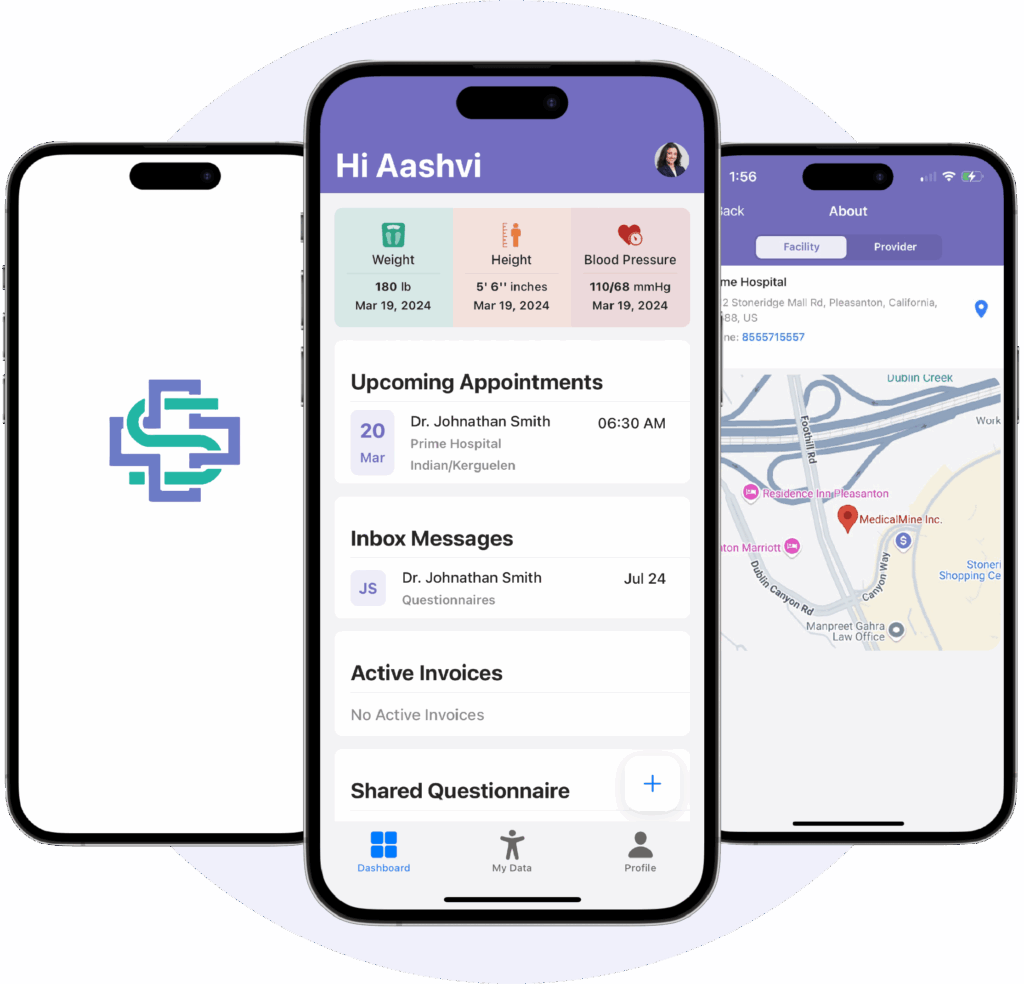
Mobile or multi-location support is crucial if your practice operates in various locations or needs on-the-go access. Ensure the software offers a mobile app or web access. Test the software on different devices to see how it performs and whether it meets your location needs.
How to Choose Practice Management Software: A 5-Step Framework
Choosing the right practice management software can simplify your operations and boost efficiency. Focus on aligning the software with your team's needs and goals. Here's a step-by-step guide to help you make an informed decision:
Step 1: Identify Your Needs
Start by defining your team's needs as the first step in selecting practice management software. Here's how to get started:
Gather Input from Stakeholders
Get feedback from key stakeholders like HR, finance, leadership, IT, and your team. Their input helps paint a full picture of what’s needed. Consider setting up a meeting or sending out a survey to gather insights. Ask about current challenges and what improvements they'd like to see.
List and Prioritize Pain Points
Identify and list the pain points or blockers in your current system. Look for issues like scheduling conflicts, billing errors, or data access problems. Prioritize these based on how often they occur and the impact on your operations. Focusing on top pain points will guide your software criteria.
Align with Policies and Goals
Ensure your software requirements align with internal policies, vendor preferences, security protocols, and regulatory goals. Check for compliance needs like HIPAA if relevant. This helps narrow down your options to those that fit your practice's framework.
Differentiate Must-Have Features
Separate must-have features from nice-to-have ones. Must-haves might include appointment scheduling, billing automation, and secure patient data access. Nice-to-haves could be mobile access or extra customization options. This list helps focus on what's essential during evaluation.
Ask These Questions:
- What complaints or blockers come up most often?
- What needs aren’t being met today?
- What features would solve your top 3 pain points?
- What ROI are you expecting from this investment?
- How will the new software align with our security and compliance needs?
Step 2: Research Practice Management Software Vendors
Now, it's time to research and compare practice management software vendors. Here's how to proceed:
Conduct Vendor Scans
Start with high-level vendor scans using review sites, rankings, and case studies. These resources provide an overview of vendor reputations and user experiences. Look for patterns in feedback, such as common praises or complaints. This helps narrow down your options quickly.
Compare Based on Needs
Compare tools based on your business size, necessary integrations, or whether you prefer outsourcing versus in-house solutions. Some vendors specialize in small practices, while others cater to larger organizations. Consider how well the software integrates with your existing tech stack or if it requires building new capabilities.
Identify Key Differentiators
Identify key differentiators like implementation support, user experience, or flexibility for niche use cases. Check if vendors offer dedicated support during setup and training. Evaluate the user interface for ease of use and adaptability to your practice's specific needs.
Document Findings
Document your findings to keep track of each vendor's strengths and weaknesses. Create a spreadsheet or a simple document listing features, pricing, and notable details. This makes it easier to compare and make informed decisions later.
Ask These Questions:
- What does each tool do best?
- Does it fit your team size, budget, and stack?
- What support and documentation are available?
- How does the vendor handle updates and upgrades?
- Are there any long-term commitments or contracts?
Top Practice Management Software to Consider
Here’s my list of the top 10 practice management software options available to help you get started in your search:
Step 3: Make a Practice Management Software Shortlist and Reach Out
Narrow down your options and start conversations with potential partners. Here's how to proceed:
Shortlist Vendors
Choose 2-4 vendors based on your research to focus your efforts. Select those that best meet your needs and align with your priorities. This helps streamline the decision-making process and ensures you're not overwhelmed with too many choices.
Send an RFI or RFP
Consider sending a Request for Information (RFI) or a practice management software RFP to gather detailed information. This is useful to understand each vendor's offerings, pricing, and support. An RFI is good for initial queries, while an RFP is more detailed and formal, asking for specific proposals.
Book Demos
Book demos with your shortlisted vendors and ask focused questions. Pay attention to how the software addresses your pain points and fits your workflow. Prepare questions about features, ease of use, and customization options to maximize the demo's value.
Use Consistent Criteria
Use consistent evaluation criteria across vendors to compare them fairly. Create a checklist or scoring system based on your priorities like features, support, and cost. This helps you objectively assess each vendor and make a well-informed choice.
Ask These Questions:
- Can you walk me through a real customer story like ours?
- What support or onboarding resources do you offer?
- What features require an upgrade?
- How do you handle updates and maintenance?
- Are there any hidden fees or costs?
Step 4: Build the Business Case
Turn your vendor research into a business case your leadership team will understand and support. Here's how to proceed:
Summarize Pain Points and Outcomes
Summarize your team's pain points and the expected outcomes to demonstrate value. Highlight issues like scheduling inefficiencies or billing errors, and explain how the software can resolve them. Show how these improvements will benefit your practice in tangible ways, like reducing wait times or increasing billing accuracy.
Present Costs and Timelines
Find and present basic cost estimates and implementation timelines. Check vendor websites or contact them directly for practice management software pricing. Present this information clearly, including any setup fees and ongoing costs. Include an estimated timeline for implementation to set realistic expectations.
Articulate ROI and Risks
Articulate the ROI, efficiency gains, and the financial or operational risks of doing nothing. Calculate potential savings from improved efficiency or reduced errors. Explain the risks of sticking with your current system, like continued inefficiencies or compliance issues. This comparison helps illustrate the software's value.
Ask These Questions:
- What business problem will this solve?
- What are the risks of doing nothing?
- What are the financial and operational upsides?
- How soon can we expect to see a return on investment?
- How does this align with our long-term goals?
Step 5: Implement Your Practice Management Software and Onboard Your Users
Plan a smooth onboarding process once you've selected a practice management software vendor. Here's how to proceed:
Communicate Rollout Plan
Communicate the rollout plan clearly to all users. Share timelines, key dates, and what each team member needs to do. Use emails, meetings, or internal platforms to keep everyone informed. Clear communication helps set expectations and prepares your team for the transition.
Assign Internal Owners
Assign internal owners and points of contact for the software rollout. Designate team members who’ll oversee the implementation and address any questions. These contacts should coordinate with the vendor and provide regular updates to your team. This ensures accountability and smooth communication.
Ensure Training and Adoption
Ensure your teams complete training and adopt the tool consistently. Schedule training sessions and encourage participation. Use vendor-provided resources like tutorials or webinars. Make sure everyone understands the tool’s features and how to use it effectively in their roles.
Create Feedback Loops
Create feedback loops during rollout, including vendor resources. Encourage your team to share their experiences and any issues they encounter. Use this feedback to make adjustments and improve the process. Engage with the vendor for additional support or clarification as needed.
Ask These Questions:
- What’s the change management plan?
- Who’s responsible for roll-out?
- How will you track early success?
- What training resources are available?
- How will feedback be collected and used?
What’s Next:
If you're in the process of researching practice management software, connect with a SoftwareSelect advisor for free recommendations.
You fill out a form and have a quick chat where they get into the specifics of your needs. Then you'll get a shortlist of software to review. They'll even support you through the entire buying process, including price negotiations.



