Medical billing codes ensure that healthcare providers get paid for their services and that insurance claims for patients are processed smoothly and efficiently.
These codes play a crucial role in the healthcare reimbursement process, acting as a bridge between services provided and payment received.
Efficient use of billing codes helps streamline the claims process, ultimately leading to quicker reimbursements and more satisfied patients.
By accurately using medical billing codes, healthcare providers can maintain financial health and continue offering essential services to their communities.
Medical billing codes are the backbone of the healthcare reimbursement process, ensuring that providers receive payment for the services they deliver and that patients' insurance claims are processed efficiently.
These codes, which standardize how medical procedures, diagnoses, and supplies are recorded, play a vital role in communication between healthcare providers, insurance companies, and government agencies.
In this article, we'll explore the different types of medical billing codes, why they are crucial for accurate billing and patient care, and how they help streamline the healthcare system and integrate with popular medical billing software.
What Are Medical Billing Codes?
Medical billing codes are standardized codes used in the healthcare industry to identify and document medical procedures, diagnoses, services, and equipment for billing and insurance purposes. They are key to how medical billing works.
Proper medical billing and coding allows healthcare providers to communicate effectively with insurance companies, government agencies, and other entities involved in the reimbursement process.
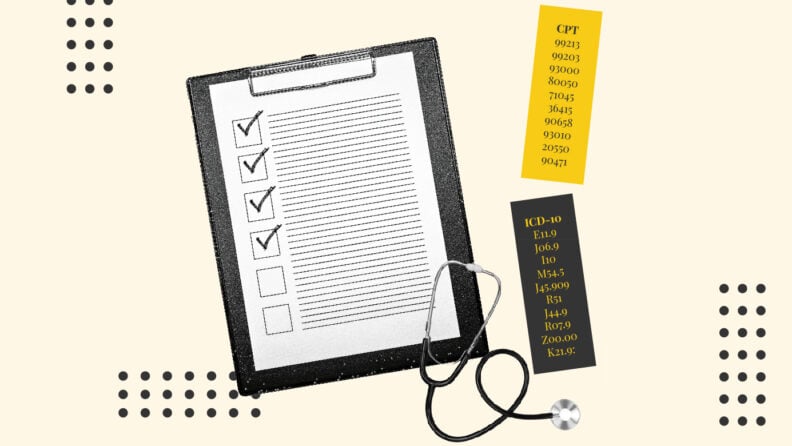
American medical billing codes are primarily organized into three categories:
- CPT (Current Procedural Terminology) for procedures
- ICD-10 (International Classification of Diseases) for diagnoses
- HCPCS (Healthcare Common Procedure Coding System) for additional services and supplies
List Of Common Medical Billing Codes
For CPT codes, there are thousands of codes describing various procedures and services, and the same applies to ICD-10 and HCPCS codes, which include an even wider range of conditions and products.
A comprehensive list would be best accessed through the official manuals or coding systems for each, such as the AMA's CPT Codebook for CPT codes or CMS for HCPCS codes.
Here’s an overview of some of the most commonly used medical billing codes in each of the 3 categories:
1. Current Procedural Terminology (CPT) Codes
These codes are used to report medical, surgical, and diagnostic procedures and services to health insurance companies.
Common CPT Codes:
- 99213: Office or outpatient visit for an established patient (Level 3).
- 99203: Office or outpatient visit for a new patient (Level 3).
- 93000: Electrocardiogram (ECG or EKG) with interpretation and report.
- 80050: General health panel, which includes multiple tests (such as CBC, CMP).
- 71045: Chest X-ray, single view.
- 36415: Collection of venous blood by venipuncture (drawing blood).
- 90658: Influenza vaccine (flu shot).
- 93010: Electrocardiogram (ECG) tracing only, without interpretation.
- 20550: Injection of substance into a single tendon sheath.
- 90471: Administration of a vaccine (per injection).
2. International Classification of Diseases, 10th Edition (ICD-10) Codes
ICD-10 codes are used to classify diagnoses, symptoms, and causes of death.
Common ICD-10 Codes:
- E11.9: Type 2 diabetes mellitus without complications.
- J06.9: Acute upper respiratory infection, unspecified.
- I10: Essential (primary) hypertension (high blood pressure).
- M54.5: Low back pain.
- J45.909: Unspecified asthma, uncomplicated.
- R51: Headache.
- J44.9: Chronic obstructive pulmonary disease (COPD), unspecified.
- R07.9: Chest pain, unspecified.
- Z00.00: Encounter for general adult medical examination without abnormal findings.
- K21.9: Gastroesophageal reflux disease (GERD) without esophagitis.
3. Healthcare Common Procedure Coding System (HCPCS) Codes
HCPCS codes are used to report medical services, procedures, equipment, and supplies not included in the CPT system. There are two levels of HCPCS codes:
- Level I: CPT codes (same as above).
- Level II: Codes for services not covered by CPT, such as ambulance services and durable medical equipment.
Common HCPCS Level II Codes:
- A0428: Ambulance service, basic life support, non-emergency.
- E0114: Crutches, underarm, other than wood, adjustable or fixed, pair.
- G0283: Electrical stimulation, unattended, for wound care.
- J1885: Injection, ketorolac tromethamine, per 15 mg (pain relief injection).
- A4253: Blood glucose test or reagent strips for home monitoring, per 50 strips.
- A7030: Full face mask used with a positive airway pressure device.
- E0601: Continuous positive airway pressure (CPAP) device.
- Q4101: Apligraf, per square centimeter (skin substitute).
- L4361: Walking boot, pneumatic and/or vacuum, with or without joints, for the ankle.
- K0001: Standard wheelchair.
Benefits Of Using Medical Billing Codes
Using these codes properly will make your medical billing process flowchart, well, flow.
Standardization and Accuracy
Medical billing codes create a standardized way to document procedures, diagnoses, and services across healthcare providers. This uniformity reduces confusion and misinterpretation, ensuring accurate communication between healthcare providers and insurers. It minimizes errors in billing and increases the likelihood of timely reimbursement.
Efficient Claims Processing
By using medical billing codes, healthcare providers can streamline the claims submission process. Insurance companies rely on these codes to quickly and correctly evaluate the services provided and issue payments. This efficiency helps reduce delays in payment and improves cash flow for healthcare providers.
Improved Patient Care Documentation
Medical billing codes help maintain accurate and detailed records of patients' medical histories and treatments. This allows providers to track patient care over time, making it easier to manage ongoing conditions and provide coordinated care. Better documentation supports continuity of care, which improves patient outcomes.
Reduced Risk of Billing Errors
Accurate use of medical billing codes minimizes the chances of billing mistakes that can lead to denied claims or underpayment. This reduces the administrative burden on healthcare providers who might otherwise spend significant time correcting errors. Proper coding ensures that claims are processed correctly the first time.
Compliance with Regulatory Requirements
Medical billing codes help healthcare providers stay compliant with legal and regulatory standards, such as those set by Medicare, Medicaid, and private insurance companies. Using these codes correctly ensures that providers follow industry guidelines, which protects them from audits and penalties. Compliance also enhances trust and accountability in the healthcare system.
Easier Data Collection and Analysis
Medical billing codes enable the collection of large amounts of healthcare data, which can be used for analysis and research. This data helps identify trends in healthcare usage, treatment effectiveness, and patient outcomes. Accurate data supports informed decision-making for both healthcare providers and policy makers.
Medical Billing Codes FAQ
What is medical billing?
Medical billing is the process of submitting and following up on claims with health insurance companies to receive payment for healthcare services provided. It involves generating medical claims using specific code sets to describe diagnoses, treatments, and procedures. The American Medical Association helps establish the CPT code set, which is commonly used in medical billing. It will often be connected to a medical payment processing system so billing and payment can be handled in tadem.
What are medical billing codes?
Medical billing codes are standardized codes used to document healthcare services, procedures, and diagnoses. These codes, such as ICD-10-CM for diagnoses and the CPT code set for procedures, ensure accurate and efficient communication between healthcare providers and insurance payers. Codes also include Category I codes, Category II codes, and Category III codes, which describe various levels of services and treatments.
Why are medical billing codes important?
Medical billing codes are essential because they ensure clarity and uniformity in the billing process. By using standardized code sets like CPT and ICD-10-PCS, healthcare providers can avoid errors, speed up claims processing, and comply with payer guidelines. Modifiers can also be applied to billing codes to provide more details about a service when needed.
What is the CPT code set?
The CPT code set (Current Procedural Terminology) is a system of codes developed by the American Medical Association that describes medical, surgical, and diagnostic services. These codes are used to report healthcare services to payers for reimbursement and are a critical part of medical billing. Each CPT code is tied to specific descriptors that clearly define the service provided.
What is the difference between ICD-10-CM and ICD-10-PCS codes?
ICD-10-CM codes are used to describe patient diagnoses, while ICD-10-PCS codes are used for inpatient procedures in hospital settings. Both sets of alphanumeric codes are important in medical billing as they ensure accurate diagnosis reporting and coding of procedures for hospital stays and surgeries.
What are Category I, II, and III codes in CPT?
- Category I codes describe procedures and services that are widely performed and approved by the FDA. These are the most commonly used codes in medical billing.
- Category II codes are supplemental tracking codes that help measure performance or quality of care.
- Category III codes are temporary codes for emerging technologies, services, or procedures.
What role do modifiers play in medical billing?
Modifiers are two-digit codes added to a CPT code to provide additional information about the performed procedure. They help clarify whether the procedure was modified or provided in a specific context, such as a different body part or unusual circumstances. Modifiers ensure that the billing accurately reflects the services provided and supports the claim with payers.
What is a fee schedule?
A fee schedule is a list of the maximum amounts a payer will reimburse for specific medical services and procedures. These fees are often tied to CPT codes or other billing codes, ensuring that both providers and insurance payers have a clear understanding of service costs.
What is the role of the CPT Editorial Panel?
The CPT Editorial Panel is responsible for maintaining and updating the CPT code set. This panel, governed by the American Medical Association, reviews and revises codes to keep up with medical advancements and ensure that the code descriptions remain relevant and accurate in the healthcare industry.
How do I use a code list in medical billing?
A code list contains all the necessary CPT and ICD-10 codes, allowing medical billers and coders to accurately document healthcare services. The list includes codes, descriptors, and modifiers to ensure the correct and efficient submission of claims to payers.
A feature of medical billing software is often integration with the codes list you will need to some extent.
Conclusion
Medical billing codes play a crucial role in helping health care professionals accurately document patient care and ensure proper reimbursement. Effective medical coding not only supports timely billing but also aids in preventive measures by tracking treatments and outcomes.
Accurate coding is essential for streamlining the billing process, ensuring appropriate follow-up care, and improving overall patient management. If the extent of medical billing and coding processes overwhelms you, you might want to consider outsourcing these tasks to a professional medical billing service.
To stay updated on the latest trends, best practices, and solutions related to your medical practice, subscribe to The Medical Practice newsletter.