Few things compare to the fulfillment that comes from healing sick or injured patients. But let’s face it—you can’t run a practice on warm fuzzies alone. And that’s the path you’re on if your patients’ bills remain unpaid.
You also need to run the business. And that’s where an understanding of medical billing and coding comes in.
In this guide, I’m diving right into the heart of this crucial field. I’ll break down all the details you need to know while equipping your specialists with an arsenal of tools and programs to kick-start their journeys.
Let’s get you and your medical team paid!
What Is Medical Billing and Coding?
Medical billing is the process of translating healthcare services into billable claims and submitting them to insurance companies for reimbursement. It involves reviewing patient records, coding medical procedures, and ensuring accurate submission of claims to minimize errors and denials—usually via medical billing software.
Medical billers work closely with healthcare providers and insurance companies to manage payments for services, track claims, and handle any disputes that may arise. The goal of medical billing is to ensure healthcare providers are properly compensated while adhering to industry regulations and payer policies.
Medical coding is the process of translating medical diagnoses, procedures, and services into standardized medical billing alphanumeric codes used by healthcare providers and insurance companies. These codes, such as ICD (International Classification of Diseases), CPT (Current Procedural Terminology), and HCPCS (Healthcare Common Procedure Coding System), ensure accurate communication between providers, insurers, and other stakeholders.
Medical coders analyze patient records, assign the correct codes, and help facilitate billing, ensuring that healthcare services are properly documented for reimbursement and statistical tracking.
You Might Also Like: What do medical billers make? Salary expectations
Medical Billing VS Medical Coding
What do medical billers and coders do? While often used together, medical billing and coding are two separate jobs.
Let’s say someone has a pounding heading and visits a doctor. The doctor orders a CT scan. A medical coder will assign specific codes representing the diagnosis (headache) and test (CT scan). If the doctor orders lab work to be done, that gets its own code, too.
After the visit has been coded, a medical biller turns it into a bill. And when the payment hits, they make sure every penny’s in its place.
In a nutshell, medical coders and billers are all about ensuring healthcare providers are correctly compensated for the services they provide.
Knowledge of State-specific medical billing deadlines is key for efficient for both medical billing and coding processes.
Medical Billing and Coding Jobs
A medical coding and billing expert helps bridge the gap between healthcare providers and insurance companies, ensuring smooth payment flows.
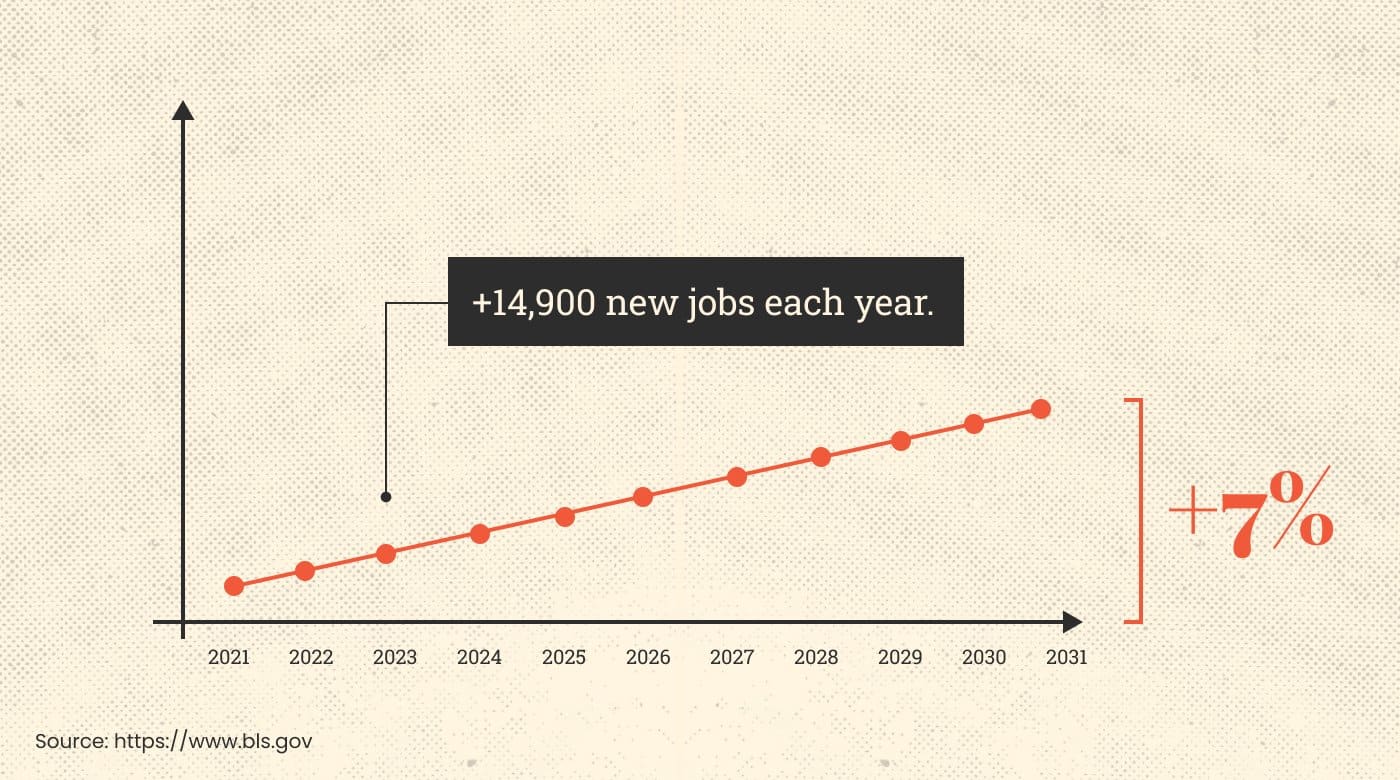
With more and more folks hitting their golden years, the demand for medical care is increasing. And as your practice grows, so does the challenge of dealing with finances.
That’s why it’s important to get a complete understanding of how the medical billing and coding field works. Your know-how will help your practice thrive.
Career Paths and Specializations
A medical billing and coding position can lead to other roles in your practice and beyond. Let’s explore the possibilities.
Certified Professional Coder (CPC): These coding experts are certified by the American Academy of Professional Coders (AAPC). CPCs often earn more than non-certified medical coders, which is something you’ll want to consider when adding one to your team.
Certified Professional Biller (CPB): Like CPCs, CPBs are certified and verified by the AAPC. They also earn more than their non-certified colleagues.
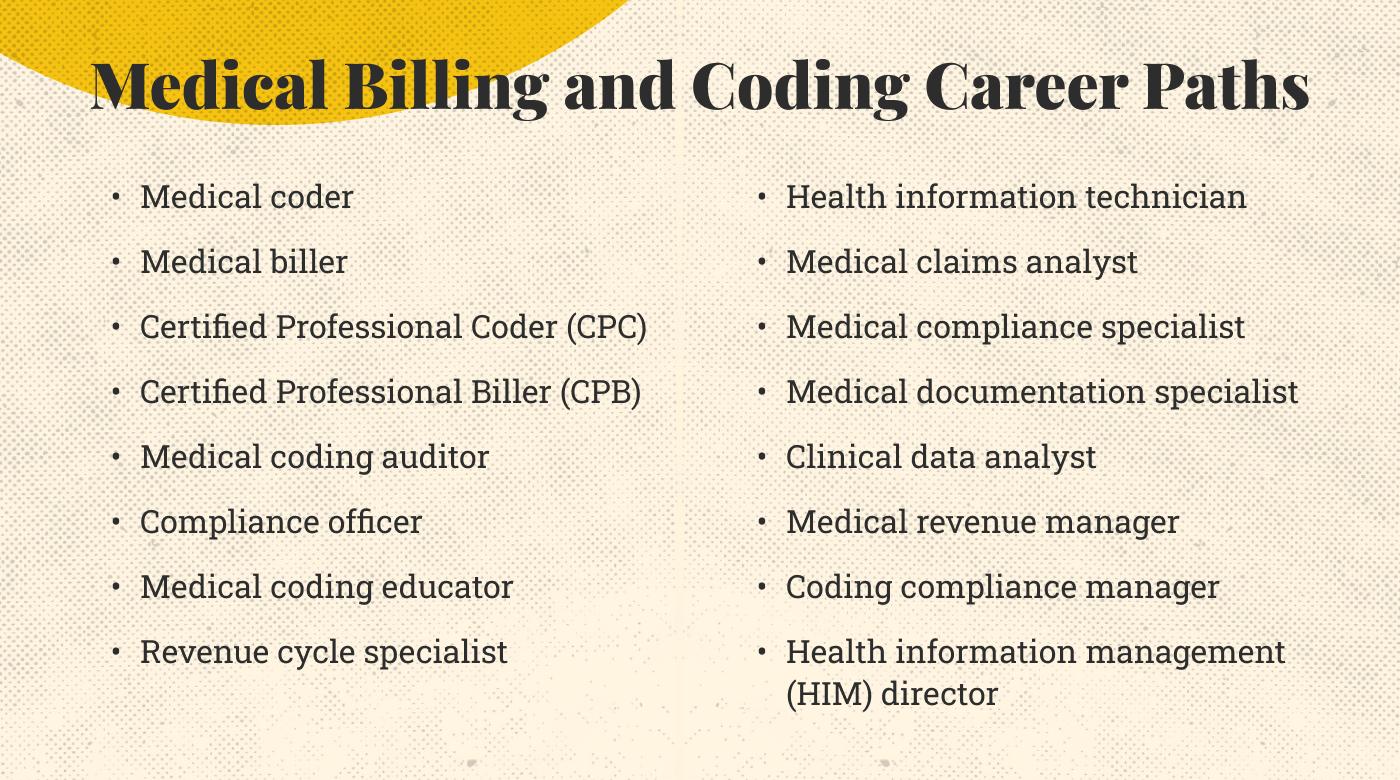
Medical coding auditor: These individuals comb through coders’ and billers’ work to make sure it’s accurate and compliant with healthcare regulations.
Compliance officer: These professionals make sure your practice is compliant with government regulations and internal policies.
Revenue cycle specialist: As their title implies, revenue cycle specialists are in charge of the practice’s revenue cycle, from patient registration and insurance verification to coding, billing and reimbursement. Ultimately, they help your team get paid.
Other roles coders and billers can dive into (with proper training, of course) include the following:
- Medical coding educator
- Health information technician
- Medical claims analyst
- Medical compliance specialist
- Medical documentation specialist
- Clinical data analyst
- Medical revenue manager
- Coding compliance manager
- Health information management (HIM) director
Additionally, hiring a specialized or more senior Medical Office Assistant might be able to help with some of these tasks.
Pay and Salary Expectations
Naturally, a medical biller and coder’s salary hinges on a variety of factors. These include your medical specialty, your location, the type of practice you’re running, and the professional’s certification status and experience.
According to a 2022 AAPC survey, specialists without certification earn an average of $46,321 per year. Their certified counterparts, however, enjoy 17.7% more, averaging $56,290.
These variables hold significant weight when you’re on the lookout for the right medical billing and coding hire for your practice.
I suggest exploring comprehensive medical billing and coding courses to gain the skills needed for efficient practice management and accurate coding.
Medical Billing and Coding Skills
Ready to find a billing and coding expert for your practice? Here’s what to keep an eye out for:
Fluency in medical terminology: Your professionals need to be fluent in medical lingo to excel in medical billing and coding. After all, how else can they flawlessly translate all the diagnoses, treatments, tests, and procedures that your doctors prescribe?

Mastery of coding systems: These systems include ICD-10-CM/PCS, CPT, and HCPCS, and I’ll dive deeper into them below.
Attention to detail: Your experts need to be detail-oriented and precise when assigning codes. One tiny coding slip can seriously affect patient care outcomes and your finances. In worst-case scenarios, the federal government can even get involved.
One endocrinologist found this out the hard way when he was fined $447,000 for billing routine blood draws as critical care blood draws.
Analytical skills: Given the complexity of medical records, billing and coding experts should be able to sift through data, spot the crucial information, and assign codes accurately.
Familiarization with coding guidelines and regulations: These include those from the American Medical Association (AMA), the Centers for Medicare and Medicaid Services (CMS), and the Health Insurance Portability and Accountability Act (HIPAA). Guidelines and regulations change all the time, so closely monitoring them is a must.
Those skills are some of the most important, but it doesn’t end there. Here are more to tick off when scouting for the perfect medical billing and coding pros:
- Tech-savviness
- Communication skills
- Ethical and professional conduct
- Time management and organization
The 3 Code Sets Specialists Must Know
The three coding systems your medical billing and coding specialists must be familiar with are:
1. ICD-10-CM
ICD-10-CM is short for International Classification of Diseases, 10th Edition, Clinical Modification. Healthcare providers across the US use this code set for diagnosis coding. It employs three to seven alphanumeric digits, consisting of a staggering 68,000 codes.
Here are some examples of ICD-10-CM codes:
J10.00: Influenza due to other identified influenza virus with unspecified type of pneumonia. Beware that only influenza A (non-novel), influenza B, and influenza C are included in this code. Other cases of influenza, such as influenza due to swine flu, are excluded and have their own codes.
J45.31: Mild persistent asthma with (acute) exacerbation. Again, some cases of asthma are included, while others are excluded, so it’s important to use the right codes for the right situations.
L70.0: Acne vulgaris. This code excludes acne keloid (L73.0).
2. CPT
CPT stands for Current Procedural Terminology. The American Medical Association (AMA) crafted it back in 1966 to standardize medical, surgical, and diagnostic services and procedures given to patients in both inpatient and outpatient settings. This system uses five alphanumeric characters, and there are roughly 10,000 codes currently in use.
Here are just a few of them:
77424: Radiation oncology treatment. For this particular code, a medical provider delivers a high dose of radiation in the form of X-rays directly to a patient’s tumor while sparing nearby healthy tissue. This is completed in a single session.
55250: Vasectomy, otherwise known as male sterilization.
80048: Basic metabolic panel (BMP). A BMP is a blood test that measures the body’s metabolism by checking on kidney function and monitoring the patient’s fluid, electrolyte, and glucose levels.
3. HCPCS
HCPCS stands for Healthcare Common Procedure Coding System, and there are two medical code sets—HCPCS Level I and HCPCS Level II.
Level I consists of the CPT code set, which I’ve outlined above, while Level II is your go-to for everything that’s not covered by Level I, such as non-physician services like ambulance rides, drugs, supplies, and equipment like wheelchairs and walkers.
This system also uses five alphanumeric digits; however, unlike CPT codes, it always begins with a letter followed by four numbers.
Let’s take a look at a few examples of HCPCS Level II codes:
A0100: Non-emergency transportation; taxi.
K0813: Power wheelchair, group 1 standard, portable, sling and solid seat and back, patient weight capacity up to and including 300 pounds. Other wheelchairs have their own codes.
M1067: Hospice services for patients provided at any time during the measurement period.
Bonus Code Set: ICD-10-PCS
ICD-10-PCS is short for International Classification of Diseases, 10th Edition, Procedure Coding System. It’s used for inpatient hospital settings only and includes seven alphanumeric digits.
Here are a few of these codes:
2W1AX6Z: Compression of right upper arm using pressure dressing.
BT39ZZZ: Magnetic resonance imaging (MRI) of kidney transplant.
GZ52ZZZ: Individual Psychotherapy, Cognitive.

Frequently Asked Questions (FAQs) About Medical Coders and Billers
Here are some additional questions and topics I wanted to cover in this complete guide to medical billing and coding.
Where Do Coders and Billers Work?
There are many places where medical coders and billers can work. The highest percentage (29%) work in hospitals, followed by physician’s offices (19%). That being said, working remotely is also on the rise.
Here’s how these three settings compare:
1. Working at a Hospital
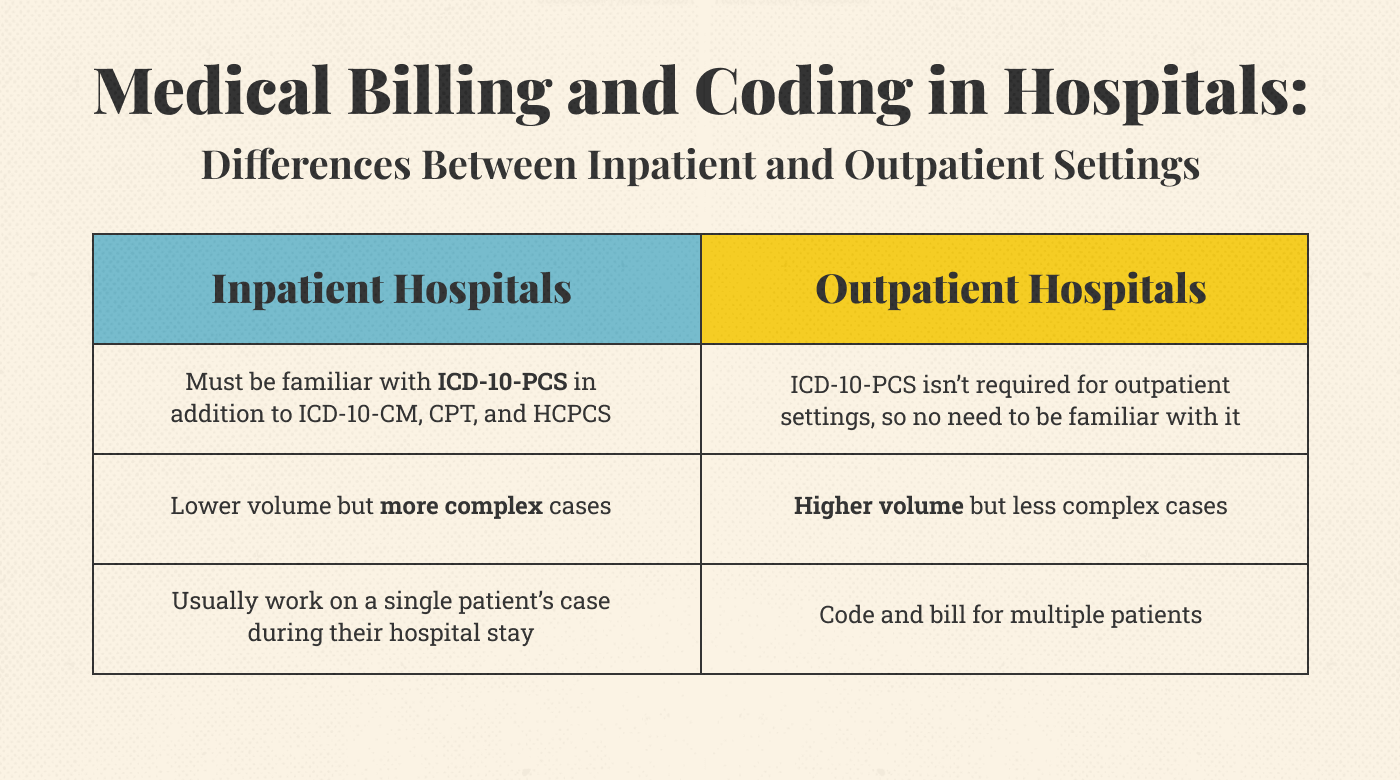
Hospitals provide both inpatient and outpatient services, and medical billing and coding look different in each of them.
Here’s a brief comparison:
Inpatient Medical Billing and Coding
Inpatient billing and coding deals with complex cases in which many healthcare services may be performed during the patient’s hospital stay.
For example, a patient who requires open heart surgery won’t just be in the hospital for the surgery itself. They may also need chest X-rays, blood tests, and an IV drip.
Details matter for inpatient coders and billers. These professionals must carefully go through medical records, surgical notes, and doctors’ notes so they can assign an accurate code to each service provided.
And that’s not all. When a patient checks in, the inpatient coder and biller must closely follow their journey, adjusting codes and billing details as the patient’s situation changes.
Inpatient medical billers and coders need a solid grip on not only ICD-10-PCS but also the other three coding sets.
Outpatient Medical Billing and Coding
Outpatient coders and billers deal with more cases than their inpatient colleagues, but those cases are usually less complex. Still, efficiency remains a key factor for success.
On a daily basis, outpatient billers and coders craft codes and put together bills for a variety of healthcare services. The challenge, then, lies in accurately assigning codes based on patients’ medical histories.
Let’s consider a patient scheduled for skin cancer removal surgery at a hospital. The coder and biller need to carefully research factors like past visits to a dermatologist and a previous skin cancer diagnosis. This knowledge helps them assign the most accurate code for the surgery.
Billing and coding in a hospital is considered advanced compared to other settings. And for good reason, since dealing with numerous different codes and handling many patients at the same time is demanding.
2. Working at a Medical Practice
A medical billing and coding specialist’s day-to-day is shaped by the unique way their practice tackles these tasks.
A family practice’s methods, for instance, will differ from those found in a therapist’s office. Still, many factors are universal for coders and billers, no matter where they work.
For instance, these professionals must all use the correct coding systems, such as ICD-10-CM for diagnoses and CPT for medical procedures. They must also use accurate codes since not doing so can result in negative healthcare outcomes and legal or financial penalties.
For instance, a psychiatrist was fined $400,000 and permanently excluded from taking part in Medicare and Medicaid. Why? Because he billed patients for 30–60-minute therapy sessions when he only provided 15 minutes’ worth of medication checks.
In some practices, billers and coders take on more than just codes and bills. They’re the go-to guys for checking up on insurance and making sure claims get sorted. And when patients have questions or concerns, these specialists step in to tackle those, too.
3. Working Remotely
Even medical coders and billers are embracing the home office. And while this arrangement offers flexibility, it also comes with risks—mostly due to the digital nature of the work.
First, at-home medical billers and coders use technology and remote tools, which means security is a big deal. Are their remote work environments meeting security standards? They’d better be since the worker is accessing sensitive patient data online.
I’m talking about medical records, coding systems, and physicians’ notes—even addresses and info for healthcare payment processing systems. That’s also why strict adherence to HIPAA guidelines and other data security regulations is so important; they are there to protect patient privacy and the confidentiality of medical info.
Working remotely often means working independently, too. While time management and self-motivation are skills all professionals should have, they’re the secret sauce for remote work. Without colleagues and supervisors around, it’s up to the individual to ensure they get their work done.

What are the Best Medical Billing and Coding Tools?
There are tons of useful tools and tech in medical billing and coding today. Understanding the categories of medical billing software is key to mastering medical billing and coding practices. Here are some you should know:
Electronic Health Record (EHR) Systems
EHR systems like Epic and Cerner integrate patient records with billing and coding. They automate documentation, making it easier for billers to extract codes and submit claims.
Medical Billing Services
Outsourcing to medical billing services like Kareo or AdvancedMD ensures claims are processed and submitted efficiently, reducing errors and improving reimbursement rates.
Medical Coding Software
Medical coding tools like TruCode and 3M Codefinder help coders assign accurate codes, improving compliance with healthcare regulations and optimizing revenue cycle management.
What Medical Billing and Coding Courses Do I Need?
As a practice manager, you want to know that your specialists are knowledgeable, and accreditation can be just the reassurance you need.
Here are a few courses that many top-notch medical billers and coders have taken to get certified:
AAPC
The AAPC created the CPC and CPB accreditations. So, when your expert is learning from them, it’s like getting knowledge straight from the horse’s mouth. And the AAPC offers even more certifications than just the CPC and CPB.
Want to specialize in cardiology? Take the Certified Cardiology Coder (CCC) certification.
Want to work in family practice instead? The AAPC also offers a Certified Family Practice Coder (CFPC) certification.
Both in-person and online training are available for all AAPC courses, and anyone who buys a course receives employment support and career advancement. And the best part of all? The AAPC boasts pass rates of 80% or higher.
Price: Packages start at $3,000
Medical Coding and Reimbursement Online Course Bundle
The American Health Information Management Association (AHIMA) offers eight credentials, including the Certified Coding Associate (CCA) and the Certified Coding Specialist (CCS). The Medical Coding and Reimbursement Online Course Bundle of 13 foundational courses prepares coders and billers for the CCA and CCS exams.
Students get one year’s access to this collection of self-paced study-at-home online courses. To sweeten the deal, they also become a member for one year after they finish the course bundle. That opens the door to perks like networking, professional development, and career guidance.
Since, according to their website, 75% of AHIMA members earn $50,000 or more, that’s a pretty good deal indeed.
Price: $2,993.25
AHIMA’s CAHIIM-Accredited Program Directory
CAHIIM stands for the Commission on Accreditation for Health Informatics and Information Management Education. Established by the AHIMA, this commission aims to closely monitor the quality of “academic programs in health information management and health informatics.”
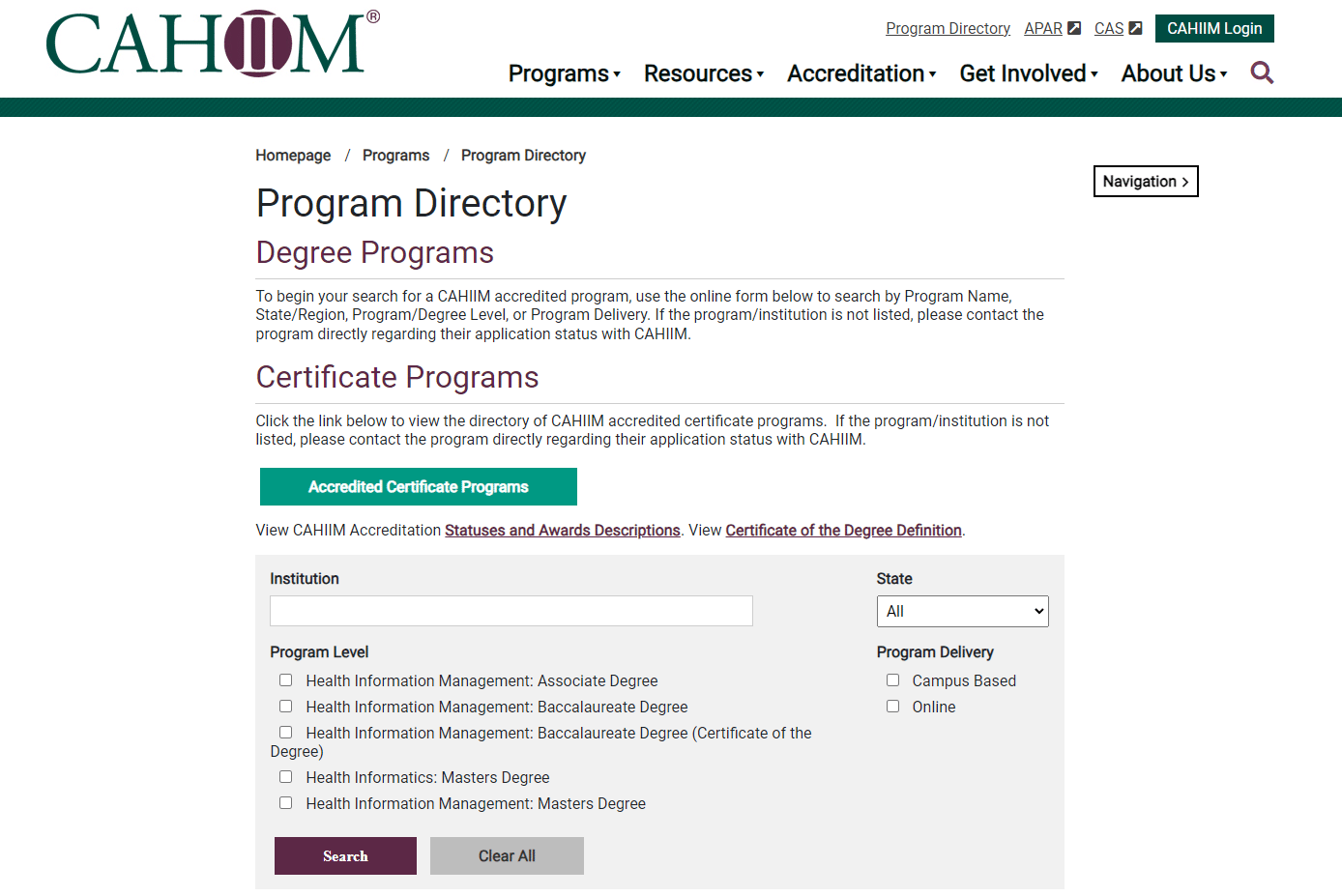
Most of the programs in this directory are academic in nature.
That’s because the AHIMA partners with several accredited schools for Registered Health Information Technician (RHIT) and Registered Health Information Administrator (RHIA) credentials. So, after completing their studies, students can take the RHIT or RHIA exam and gain a shiny new degree.
Use this directory to find an accredited school in your state.
CareerStep
CareerStep’s comprehensive online medical coding and billing program is AAPC- and AHIMA-approved, and it’s designed to sync with the CPC exam.
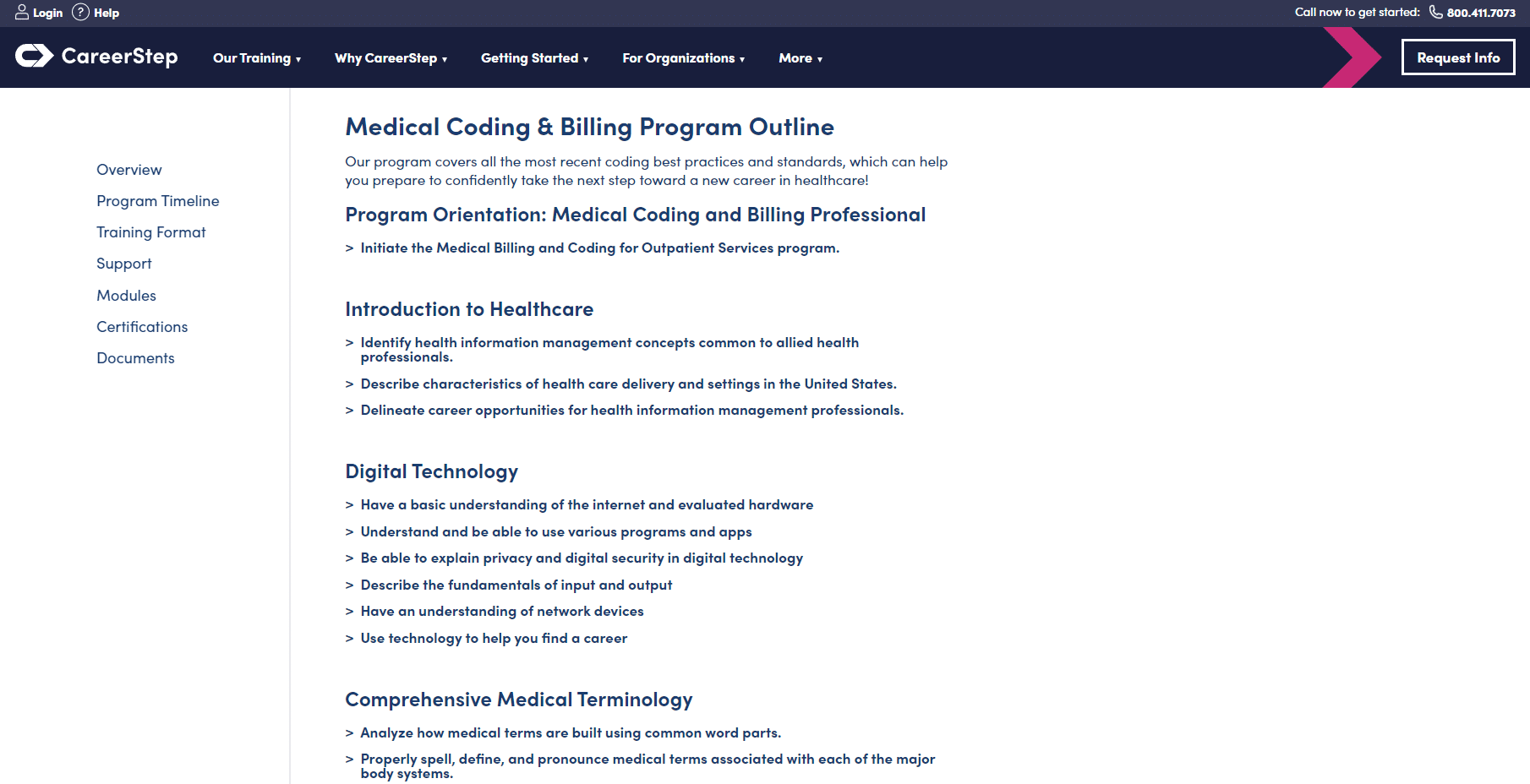
Students get a full year’s access, giving them the freedom to learn at their own pace. The program also comes with 1:1 support, along with certification prep materials and exam fees.
Price: $3,699
Certification Coaching Organization (CCO)
Billed as a local school alternative, the CCO offers a variety of medical billing and coding courses, including specializations. And yes, these courses are AAPC-approved.
All courses are online, meaning that students can set their own pace for learning. However, unlike the previous courses mentioned on this list, these courses only come with nine months’ access. While that may not be enough time for someone with a packed schedule, the shorter deadline might light a fire in determined students.
The CCO has built a thriving learning community around its courses, with student support forums, live group webinars, and certified instructor support. Students also get free access to exam preparation documents, such as mock exams.
Price: Individual courses start at $429, but specializations cost between $1,000 and $2,000.
Medical Billing & Coding FAQ
What is Medical Billing & Coding Software?
Medical billing and coding software is a tool that helps healthcare providers manage billing and insurance claims. It organizes patient data, handles medical codes for treatments, and creates invoices for insurance companies and patients.
Medical billing tool features make it easier to keep track of payments, reduces paperwork, and speeds up the process of getting payments from insurance companies, making the billing process smoother for doctors' offices and hospitals.
What makes online learning flexible for medical billing and coding?
Online learning offers flexibility by allowing students to study from home and set their own schedules. This is especially helpful for those balancing work or family commitments. Many programs are self-paced, meaning you can progress at your own speed while still accessing all course materials and support.
Do medical billing and coding programs offer employment support?
Yes, most reputable programs provide career support, including resume assistance, job placement services, and networking opportunities. Some even connect students with potential employers or offer internships to gain hands-on experience, helping ease the transition into the workforce.
What does the program structure and curriculum look like?
Medical billing and coding programs typically include courses on healthcare systems, medical terminology, coding systems like ICD and CPT, and healthcare laws. The structure often combines reading materials, lectures, and practical coding exercises to help students understand both theory and practice.
Why is accreditation important for medical billing and coding programs?
Accreditation ensures that the program meets industry standards for quality education. Attending an accredited program is crucial because it makes students eligible for certifications and often improves job prospects. Employers also prefer graduates from accredited programs, knowing they have received proper training.
Are there continuing education opportunities in medical billing and coding?
Yes, continuing education is essential for medical billing and coding professionals to stay up-to-date with changes in coding systems, healthcare laws, and technologies. Many organizations offer courses, seminars, or certifications that help professionals maintain their credentials and enhance their skills.
Are there degree programs for medical billing and coding?
While many people pursue a certificate, there are also degree programs, such as associate’s degrees, which provide a more comprehensive education. These programs often include general education subjects along with specialized training in billing and coding, offering broader career opportunities.
Build the Best Medical Billing and Coding Team
With a medical biller and coder on your side, you have the tools and skills you need to boost your practice’s success—in both its mission and its bottom line.
Embracing this strategic field means you’re not just securing your practice’s financial health—you’re making a huge impact on those you serve. You’re in a better position to heal, uplift, and create lasting change.
To stay updated on the latest trends, best practices, and solutions related to your medical practice, subscribe to The Medical Practice newsletter.
Now go forth, heal, and prosper!